A team of researchers from Cornell University has made significant strides in understanding how psilocybin, the active compound found in magic mushrooms, interacts with the brain to potentially alleviate depression. By combining psilocybin with a variant of the rabies virus, the researchers have mapped the alterations in brain connectivity that occur following treatment. Their findings were published in the journal Cell on December 5, 2023.
The study, led by postdoctoral researcher Quan Jiang and senior author Alex Kwan, a professor of biomedical engineering at Cornell, aimed to identify how psilocybin reshapes neural circuits associated with negative thinking. The researchers discovered that psilocybin weakens cortico-cortical feedback loops, which may contribute to the cycle of negative rumination often experienced by those suffering from depression. Additionally, the compound appears to enhance connections between sensory processing areas and subcortical regions, potentially improving sensory-motor responses.
In previous research, Kwan’s group demonstrated that a single dose of psilocybin can induce structural plasticity in the brain by promoting the growth of dendritic spines. This latest investigation builds on that work by exploring the specific brain regions affected by psilocybin treatment. Kwan noted, “A lot of people were excited about the earlier study, because psychedelics are promising therapeutics but we don’t know why they work. Our study showed that the rewiring in the brain lasts a long time.”
To map the brain’s connectivity, the researchers utilized a unique approach that involved the rabies virus, engineered by collaborators at the Allen Institute for Brain Science in Seattle. This virus can traverse synapses, effectively charting the brain’s intricate wiring. Kwan described this process as similar to using mapping technology to explore a neighborhood’s streets. “With psilocybin, it’s like we’re adding all these roads to the brain, but we don’t know where the roads go,” he explained.
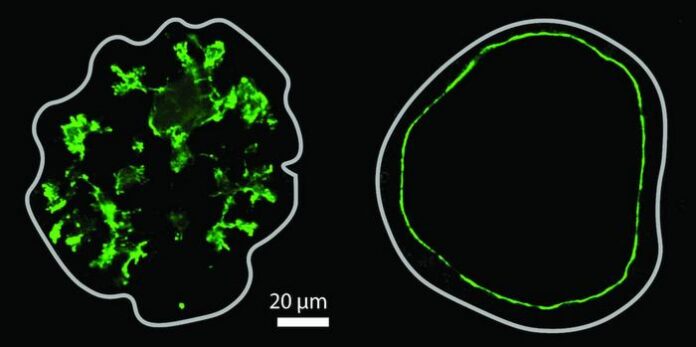
The experimental procedure began with the injection of psilocybin into a mouse’s frontal cortical pyramidal neurons. A day later, the researchers introduced the rabies virus, which labels connected neurons with fluorescent proteins. After a week of incubation, the team compared the brains of treated mice to control mice that had only received the virus. The results indicated that psilocybin diminished the strength of recurrent connections within the cortex, highlighting the potential for the substance to disrupt negative thought cycles.
Kwan stated, “Rumination is one of the main points for depression, where people have this unhealthy focus and they keep dwelling on the same negative thoughts. By reducing some of these feedback loops, our findings are consistent with the interpretation that psilocybin may rewire the brain to break, or at least weaken, that cycle.”
Further observations revealed a more robust connection between sensory areas of the brain and subcortical regions. Initially expecting to find limited connections, Kwan was surprised to discover that psilocybin’s effects spanned the entire brain. “This is really looking at brain-wide changes,” he remarked, emphasizing that this research opens new avenues for understanding the therapeutic potential of psychedelics.
The study’s findings also suggest that the level of neural activity may influence how psilocybin rewires brain circuitry. By manipulating activity in specific brain regions, the researchers propose that it may be possible to enhance positive plasticity while minimizing negative effects. “That opens up many possibilities for therapeutics, how you maybe avoid some of the plasticity that’s negative and then enhance specifically those that are positive,” Kwan concluded.
Co-authors of the study included Ling-Xiao Shao, Amelia D. Gilbert, Jack Nothnagel, Neil Savalia, and Pasha Davoudian from Yale University; Shenqin Yao and Hongkui Zeng from the Allen Institute; Guilian Tian and Kevin Beier from the University of California, Irvine; and Tin Shing Hung and Hei Ming Lai from the Chinese University of Hong Kong. The research received support from One Mind and the National Institutes of Health.
This innovative research not only sheds light on the therapeutic mechanisms of psilocybin but also paves the way for future studies aimed at developing effective treatments for depression and related mental health conditions.