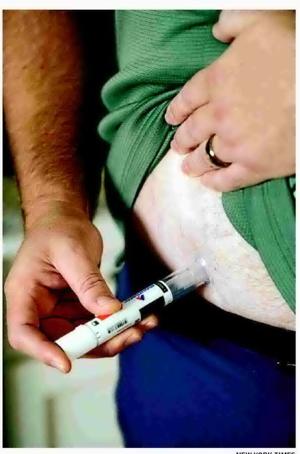
Recent findings from a clinical trial have cast a shadow over the previously celebrated image of Ozempic, a medication primarily used for treating Type 2 diabetes. The drug, which has garnered attention for its potential benefits beyond blood sugar management, now faces scrutiny following its performance in a trial aimed at assessing its effects on dementia.
Trial Results Raise Concerns
The trial, conducted by a team of researchers, aimed to explore whether Ozempic could provide cognitive benefits in dementia patients. Results released in early March 2024 indicated that the drug did not demonstrate significant improvements in cognitive function or memory retention compared to a placebo. This outcome contradicts earlier assertions suggesting that Ozempic might have neuroprotective properties, which had contributed to its “miracle” status among some advocates.
According to the researchers, the study involved a diverse group of participants aged 60 and older, with varying degrees of cognitive impairment. Lead investigator Dr. Emily Thompson, a neurologist at the National Institute of Health, stated, “While we have seen promising results in other health areas, these findings indicate that Ozempic may not offer the cognitive benefits we hoped for in dementia patients.”
Impact on Market Perception
The implications of these findings are significant for both the medical community and the pharmaceutical market. Ozempic’s manufacturer, Novo Nordisk, has enjoyed a surge in popularity due to its perceived multifaceted benefits, including improvements in liver, kidney, and heart health. As of now, the company’s stock has shown fluctuations in response to the trial results, reflecting investor concerns about the drug’s future applications.
Analysts have noted that the hype surrounding Ozempic could lead to a reassessment of its efficacy in treating conditions beyond diabetes. According to a report from Market Research Future, the global diabetes medication market is projected to reach $100 billion by 2025, but the recent trial may alter growth expectations for drugs like Ozempic that were previously seen as potential blockbusters.
The results have also prompted calls for more comprehensive research into the long-term effects and potential risks associated with Ozempic. Experts are urging caution among healthcare providers when prescribing the drug for off-label uses, especially in vulnerable populations such as those with cognitive impairments.
As the medical community absorbs these revelations, patients and healthcare providers alike are left to navigate the complexities of treatment options in light of new evidence. The ongoing discourse surrounding Ozempic serves as a reminder that scientific advancements can yield both promise and disappointment, underscoring the importance of rigorous clinical trials in evaluating the true impact of medications.
In summary, while Ozempic has proven beneficial for managing Type 2 diabetes and improving cardiovascular health, its recent trial has raised questions about its role in dementia care. The findings not only affect patient treatment plans but also challenge the broader narrative of the drug’s versatility in addressing multiple health concerns.