Research has revealed that spending less time in two critical stages of sleep may significantly increase the risk of developing Alzheimer’s disease. According to findings discussed by Dr. Brianne Miner from Yale School of Medicine, individuals who experience reduced periods of deep sleep and REM sleep may face cognitive decline years later.
In a segment aired on the Broadcast Retirement Network, host Jeffrey Snyder engaged Dr. Miner in a conversation about the intricate relationship between sleep patterns and Alzheimer’s disease. The discussion highlighted how sleep is not merely an extended period of rest; rather, it involves cycling through multiple stages, each with unique characteristics and functions.
Understanding Sleep Stages and Their Importance
Dr. Miner explained that typical sleep consists of four phases that individuals cycle through 4 to 6 times each night. These phases include lighter stages of sleep (N1 and N2) followed by deeper sleep (N3). The first REM (rapid eye movement) sleep period occurs approximately 90 minutes after falling asleep, during which dreaming typically takes place. Each of these stages plays a vital role in maintaining overall health and cognitive function.
The study, led by postdoctoral fellow Dr. Cho, aimed to explore how specific sleep stages relate to the onset of Alzheimer’s disease. Dr. Miner noted that while it is already established that sleep impairments contribute to the risk of Alzheimer’s, their research sought to pinpoint which sleep stages are most crucial.
Dr. Cho’s findings indicated that individuals who spent less time in deep sleep (N3) and REM sleep were more likely to exhibit brain changes associated with early Alzheimer’s. Specifically, areas of the brain known to be affected early in the disease process were smaller in those who lacked sufficient time in these vital sleep stages.
Age-Related Changes in Sleep Patterns
As people age, their sleep patterns often change. Dr. Miner remarked that many older adults report difficulties in achieving prolonged periods of restorative sleep, which can lead to cognitive challenges. She emphasized that it is normal for older individuals to experience shorter sleep durations and increased night-time awakenings.
The recommended amount of sleep for adults remains around seven hours per night. Dr. Miner pointed out that if someone is consistently getting only six hours of sleep, it may warrant further investigation to identify potential sleep disorders or other underlying issues affecting sleep quality.
When discussing the potential benefits of napping, Dr. Miner explained that short naps can indeed help mitigate the effects of inadequate overnight sleep. While some studies suggest that excessive napping may be linked to adverse health outcomes, brief daytime naps can enhance cognitive performance and support cardiovascular health, especially for those not receiving enough sleep overnight.
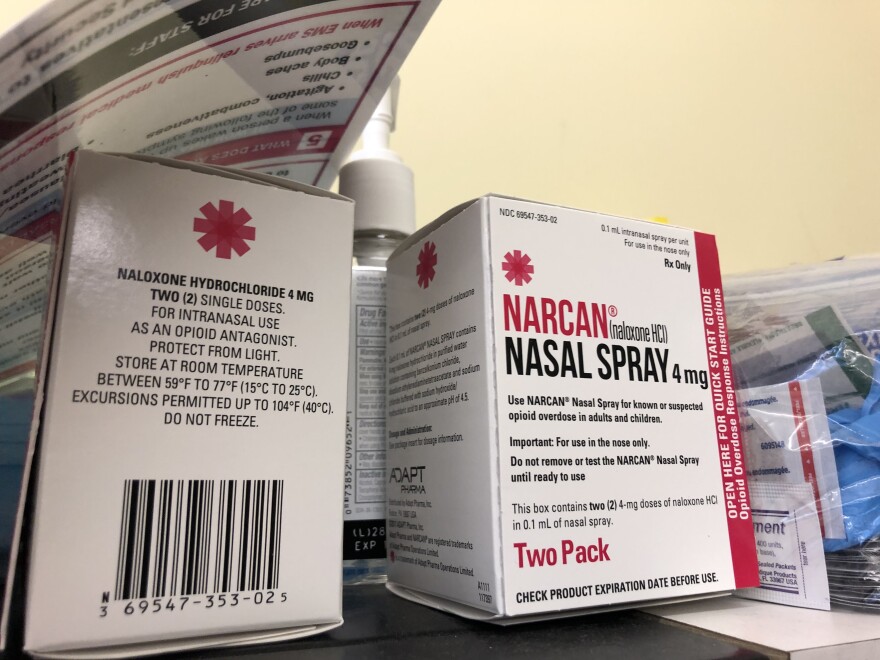
Seeking Help for Sleep Issues
Individuals experiencing persistent sleep challenges are encouraged to consult their primary care providers. Dr. Miner advised that discussing sleep issues with a doctor is a crucial first step in determining if a referral to a sleep specialist is necessary.
In terms of improving sleep hygiene, Dr. Miner suggested several practical strategies that do not require expensive investments. Maintaining a consistent sleep schedule, avoiding caffeine and alcohol in the hours before bedtime, and engaging in regular physical activity can all help enhance sleep quality.
Dr. Miner noted that while some individuals may consider high-end mattresses or sleep aids, many effective solutions are accessible and cost-effective.
The discussion concluded with Dr. Miner emphasizing the importance of awareness around sleep as a vital component of health, particularly as it relates to aging and cognitive function. By prioritizing good sleep practices, individuals may significantly improve their quality of life and potentially reduce the risk of Alzheimer’s disease.