Scientists at the University of California, San Francisco (UCSF) have developed a revolutionary approach that reimagines fat cells as potential allies in the fight against cancer. This innovative strategy involves genetically engineering ordinary white fat cells to act like energy-burning beige fat cells, enabling them to compete with tumors for vital nutrients. The findings, published in the journal Nature Biotechnology on February 4, 2024, showcase how modified fat cells can significantly reduce tumor growth in preclinical models.
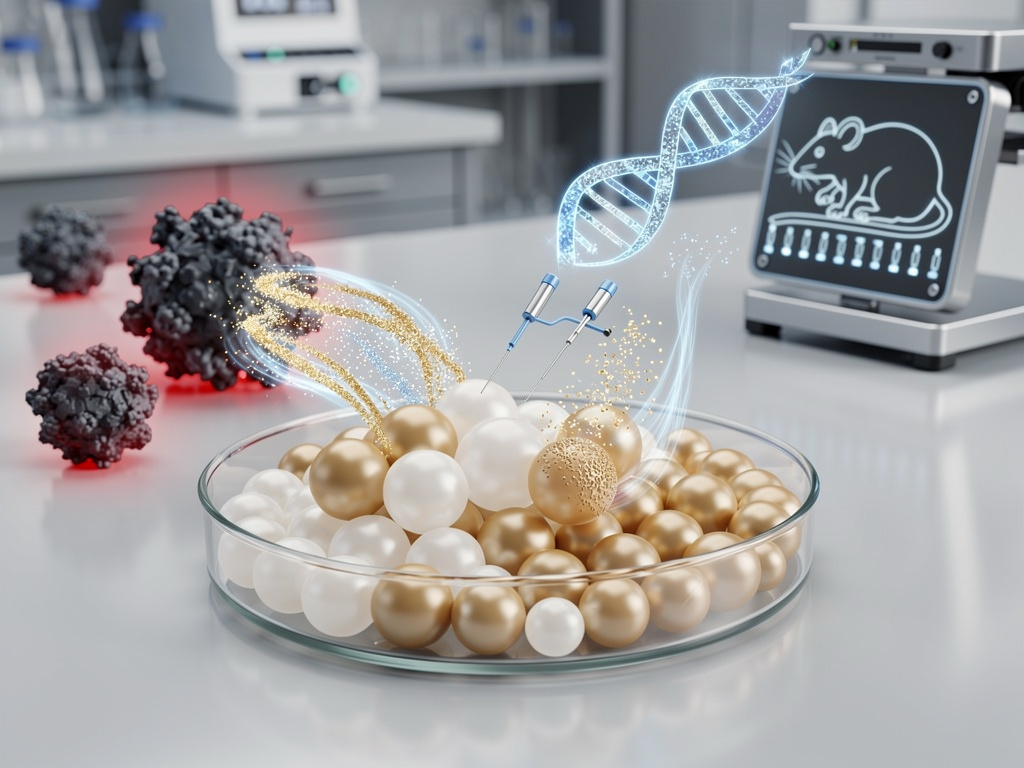
By utilizing CRISPR gene-editing technology, the research team, led by Professor Nadav Ahituv, has successfully activated genes that convert sluggish white fat into hyperactive beige fat. These engineered cells, when implanted near tumors in mice, aggressively absorb nutrients such as glucose and fatty acids, effectively starving tumors of their essential resources. Early experiments demonstrated promising results across various cancer types, including breast, prostate, and colon cancers, with some tumors shrinking dramatically or even disappearing completely without damaging surrounding healthy tissue.
With traditional treatments like chemotherapy and radiation often resulting in severe side effects, the UCSF method offers a novel alternative by exploiting the metabolic needs of cancer cells. These cells thrive by rapidly consuming nutrients, and the engineered fat cells turn this advantage against them. Early data indicate that the modified cells can reduce tumor sizes by up to 80%, significantly extending survival rates in mice.
From Liposuction to Targeted Therapy
The inspiration for this research stems from observations in cosmetic surgery, where fat grafts are routinely used for reconstructive purposes. Researchers at UCSF speculated whether these cells could be repurposed as a weapon against cancer. By implanting modified fat near tumor sites, they created a competitive environment that favored the nutrient-hungry beige fat.
Electron microscopy images provided by UCSF illustrate how these fat organoids successfully outcompete tumors for nutrients, resulting in depleted nutrient zones around cancer masses. Previous attempts to starve tumors metabolically, such as using drugs to inhibit glucose uptake, have often failed due to the body’s compensatory mechanisms. The UCSF approach introduces an external competitor, thereby sidestepping these challenges.
With the backing of the National Institutes of Health, ongoing refinements are underway. The research team aims to ensure that the engineered cells do not migrate or cause unintended metabolic imbalances, key concerns as they move toward clinical trials.
Addressing Regulatory and Ethical Considerations
As this innovative therapy advances, it will undergo rigorous scrutiny from regulatory bodies like the FDA, particularly regarding safety profiles and potential off-target effects associated with CRISPR technology. While Ahituv’s team reports high specificity in their models, the implications of gene editing will require careful monitoring as the research progresses.
Public sentiment regarding this breakthrough has been mixed, with excitement tempered by caution. Social media discussions reflect a blend of enthusiasm for its potential and skepticism about the challenges ahead. Industry experts suggest that successful human trials could disrupt the estimated $200 billion oncology market, paving the way for new therapeutic avenues.
The implications of this research are vast. Integrating engineered fat cells with existing treatments could revolutionize cancer care. For instance, post-surgical fat implants might help prevent recurrence, while injectable engineered cells could target hard-to-reach tumors.
The vision for the future is clear: to harness the power of fat cells, often viewed as mere storage, transforming them into agents of healing. As Ahituv’s team continues its work, collaborations with institutions like the National Cancer Institute are expected to accelerate the translation of these findings into clinical applications.
Overall, this innovative approach not only highlights the potential of metabolic manipulation in cancer treatment but also suggests a new paradigm where fat cells become crucial players in the battle against one of medicine’s most persistent challenges.